ALPA offers a Great Tool in the Pilot Mental Health Struggle
The Air Line Pilots Association has issued a very useful guide for its members to self-evaluate tool (“IMSAFE”) as a predicate to taking the controls. As part of its recommendation, ALPA informs these men and women who work in the cockpit that the union has made available a PILOT PEER SUPPORT group.
Although a number of strategies have been floated to address this dilemma, what seems to provide the greatest (in coverage and over time) is some form of PPS. This safety risk management tool should be applied to all aviators as made clear by the below recitation of aeromedicine’s tortuous search for answers.
The Aeromedical Profession faces a number of complex challenges. The difficulty of diagnosis increases when the symptoms may not be constantly evident to the individual and/or health professionals and even more elusive, the indicia of a problem, even when present, may not be detectible even under standard tests. With PILOT MENTAL HEALTH subjective analyses—based on patient input and clinician judgment—remain essential for accurate mental health diagnosis.
The JDA Journal has covered this enigmatic problem for years and here is a sampling of those posts:
A second ARC on Pilot Mental Health emphasizes DISCLOSURE WITHOUT REVOCATION: what does that mean? April 8, 2024
With contentious debate, a 25 year professional’s pilot mental health insights March 18, 2024
Differing views about FAA mental health policy February 14, 2024
Alaska jump seat Pilot Incident suggests that Pilot Peer Groups for Mental Health should be MANDATORY to detect this insidious safety risk. October 24, 2023
In 2017 and thereafter, PILOT MENTAL HEALTH has benefitted from the education, experience, and expertise of Dr. Susan E. Northrup was named the Federal Air Surgeon for the U.S. Federal Aviation Administration. She has been instrumental in advancing the FAA’s policies and procedures applicable to the members of the cockpit. The DILEMMA is on one hand:
- PILOTS, who need help, are reluctant to seek it, because admitting to having an issue leads to their ineligibility to fly

And on the other hand—
- Without a safe path to treatment, PILOTS, not being treated, are STILL LIKELY to attempt to enter the cockpit at GREAT RISK to all
Here is a short list of recent FAA actions and pronouncements on this predicament:
FAA Launches Rulemaking Committee On Pilots’ Mental Health November 9,2023
Mental Health & Aviation Medical Clearances Aviation Rulemaking Committee- Recommendation Report April 1, 2024
FAA PUBLISHES MENTAL HEALTH RECOMMENDATIONS April 3, 2024
The most recent recommendations from the April 2024 ARC sets that’s as priorities:
A summary of the ARC’s Recommendations is below:
• Create a non-punitive pathway for disclosing mental health conditions and treatments;
• Revise and evaluate the requirements for reporting and certification/qualification of psychotherapy (talk therapy), depression/anxiety; attention deficit hyperactivity disorder, and post-traumatic stress disorder;
• Ensure that aeromedical screening protocols and requirements are based on Safety Management System principles (i.e., proportionate, relevant, and risk-based), and appropriately communicated to applicants;
• Expand the use and promotion of Peer Support Programs.

• Develop mental health literacy, education, and awareness campaigns;
• Increase mental health training and improve quality assurance for Aviation Medical Examiners (AMEs);
And
• Modernize the FAA’s information management system/Aviation Medical Certification Subsystem.
None of these is mutually exclusive and all should be initiated. However, the ALPA PPS (ARC’s term PDP) provides a more pervasive and thus hopefully effective tactic to reduce this risk.
- Members of a PPS are given significant training in identifying symptoms and other cockpit professionals should also learn these behaviors. WHY? Because recognizing these signals is most effective when they are at work. An AME or psychiatrist may assess an ATP at a point in time when their patient is not suffering from stress. A pilot, who was deemed fit for flying a month ago, may have encountered a distressing problem that could impact performance on reporting for duty. Mental Health is not constant; the degree of impact varies over time.
- This training and awareness increase the likelihood that an intervention may be more salubrious. There are strategies—verbal (word choice), body language, counseling skills, and empathy—that will aid in the detection and in supporting the seeking of help.
THANK YOU ALPA for designing this model PPS.

+++++++++++++++++
On this page: Self-Evaluate | Get Help | Podcast | Resources

SELF-EVALUATE
Something every airline pilot should ask themselves before stepping onto an airline flight deck: “AM I IN THE GREEN?” The question is a reference to the IMSAFE checklist, a self-assessment tool for pilots to determine physical and mental wellness in preparation for each flight. The six-letter acronym stands for illness, medication, stress, alcohol, fatigue, and emotion.
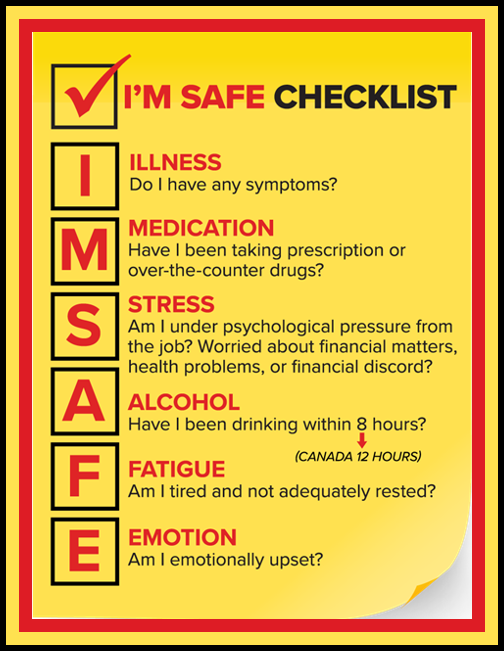
The last evaluation component, emotion, addresses mental wellbeing, and the colors of the Mental Health Continuum help you gauge the state of your mental health based on your attitude, behavior, and adherence to certain social norms.
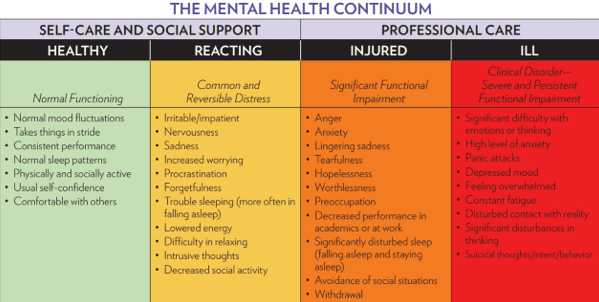
Self-evaluation is critical. So . . . Are you in the green? If the answer is “no,” ALPA’s Pilot Peer Support (PPS) program is available if and when you need help.
Regulators in the United States and Canada are taking a MORE PROGRESSIVE AND TRANSPARENT APPROACH TO MENTAL HEALTH ISSUES in aviation and recognize that, in many cases, the key to recovery is early intervention through peer programs like PPS.
What Is PPS?

PPS is a network of pilot volunteers who help fellow ALPA members deal with stress from any source—financial concerns, family or relationship problems, or any other work or personal issues. PPS volunteers are available to listen and offer confidential, nonjudgmental support to ALPA members in the United States and Canada.

.+++++++++++++++++++++++++