What can Health Care learn from Aviation’s SMS ?


AVIATION SAFETY is the foremost thought for all who work in this demanding field. The introduction of Safety Management Systems into our work has refined the industry’s ability to address risks. Not all of our colleagues have found this new discipline to their liking—too much paperwork, time-consuming, damming records are among the complaints. These nattering nabobs of negativism justify their critique because they do not see the benefits. The holders of this view may not have experienced the previous approach insultingly, but unfortunately aptly, named “tombstone” aviation response. For decades, a new rule resulted from a recent accident or incident. Not so with SMS which provides a discipline to be proactive.
A recent article from a medical journal provides some comparative comments that might reduce that antagonism. MULTIPLE EXPERTS FROM THE HEALTH CARE SECTOR ARE SO ENAMORED BY AVIATION’S SUCCESSES THAT THEY CHASTISE THEIR COLLEAGUES FOR FAILING TO ADOPT our advanced TO IMPROVE THEIR PROFESSION, SAVING LIVES. Such praise should reduce or eliminate the doubts about SMS’ benefits.
A summary of the aspects of aviation safety culture’s advances is informative:
- Checklists
- Open, equal communications within the cockpit
- End of the “name, blame, shame, retrain,” pattern instead learning from mistakes
- Institution of JUST CULTURE as the philosophy to prevent repetition of the same human error
- Use of a BLACK BOX to provide a factual basis for enhancing patient safety
- Collection and analysis of all the elements of flight to look for trends, actions which may inadvertently precede a problem to find a better technique
- Sharing best practices and developing standardization
Those who have been in the aviation QC/QA business for the past decade may have taken these points for granted. In retrospect, aviation should take credit, for example. for the CVR/FDR’s contribution to enhancing safety. Reading the paper below will reinforce our collective flight self-esteem.
The Doctors did well, but there may be more to stitch up this transplant operation. A few points, ideas which professionals with extensive SMS experience might help apply to the hospital context:
- One of the most aspects of SMS is that all who are part of an organization MUST be aware of safety 27/7/365 and must be allowed to engage in the pursuit of enhancing passengers’ (patients’) protection. The apparent hierarchical nature of hospitals, in particular the surgery theater, deflates the contributions of attendings, nurses and others considered not the Alpha person. IF TRUE, equality must be established in terms of safety vigilance/contribution.
- Though the various examples mention communications, SMS thrives on DIALOGUE, DEBATE & DISCOURSE. Critical to finding a real consensus solution is the contribution by everyone in the health care system; an HR specialist, for example, might see that the critical measurement in a procedure requires above average vision—simple response: making sure that this step is performed with precision—hospital providing all employee regular eye testing and free eyeglasses as a benefit. Cheaper than a multimillion-dollar PI payment and immediate improvement in patient safety.
- A similar aspect of SMS that one, who has worked through the process multiple times, recognizes and will incorporate into the health organization’s permanent ethic is that the identification of the safety priorities, the prioritization of risk responses and design of solutions have an institutional value. The active participation of all the organization’s major functions on the Safety Risk Management usually results in broader support for the solution selected. Having debated the relative merits, the individuals know the values of the selected option. Late night budget sessions have known to be sites for killing a “pet project.” The SRM members know the why’s and wherefores.
- Rich sources for SMS consideration include VSRP, ASAP, FOQA and other data collections. The numbers are relevant on an internal basis- e.g., carrier X has seen cracks in a specific disk, but also turbines on a number of engines have had small flaws which accumulate to a higher warning level. Those resources are maintained by NASA, the FAA and other independent organizations. The US and world medical sectors need to copy this capacity.
SMS is not an easy panacea; to truly advance the wellbeing of the passengers/patients, thoughtful process and inspired participation maximize its value above the time dedicated to the cause. Lifting the involvement of all begins with someone who has seen what can be achieved. We’re here to help.

—————————————————————————————————-
Healthcare wants to fly as high as the aviation industry. Can it?
Paige Twenter – Monday, October 30th, 2023

Hospital executives often rave about aviation’s success in dramatically lowering the number and scope of accidents over the last 50 years — but when it comes to vastly improving safety, the healthcare industry has failed to leave the runway.
Other than medical facilities and airplanes, there aren’t many places where a small error can lead to numerous fatalities. Thus, healthcare leaders have long been looking up to aviation. In 2007, ATUL GAWANDE, MD, wrote a popular article in The New Yorker that highlighted why hospitals should adopt the aviation industry’s heavy reliance on safety checklists.
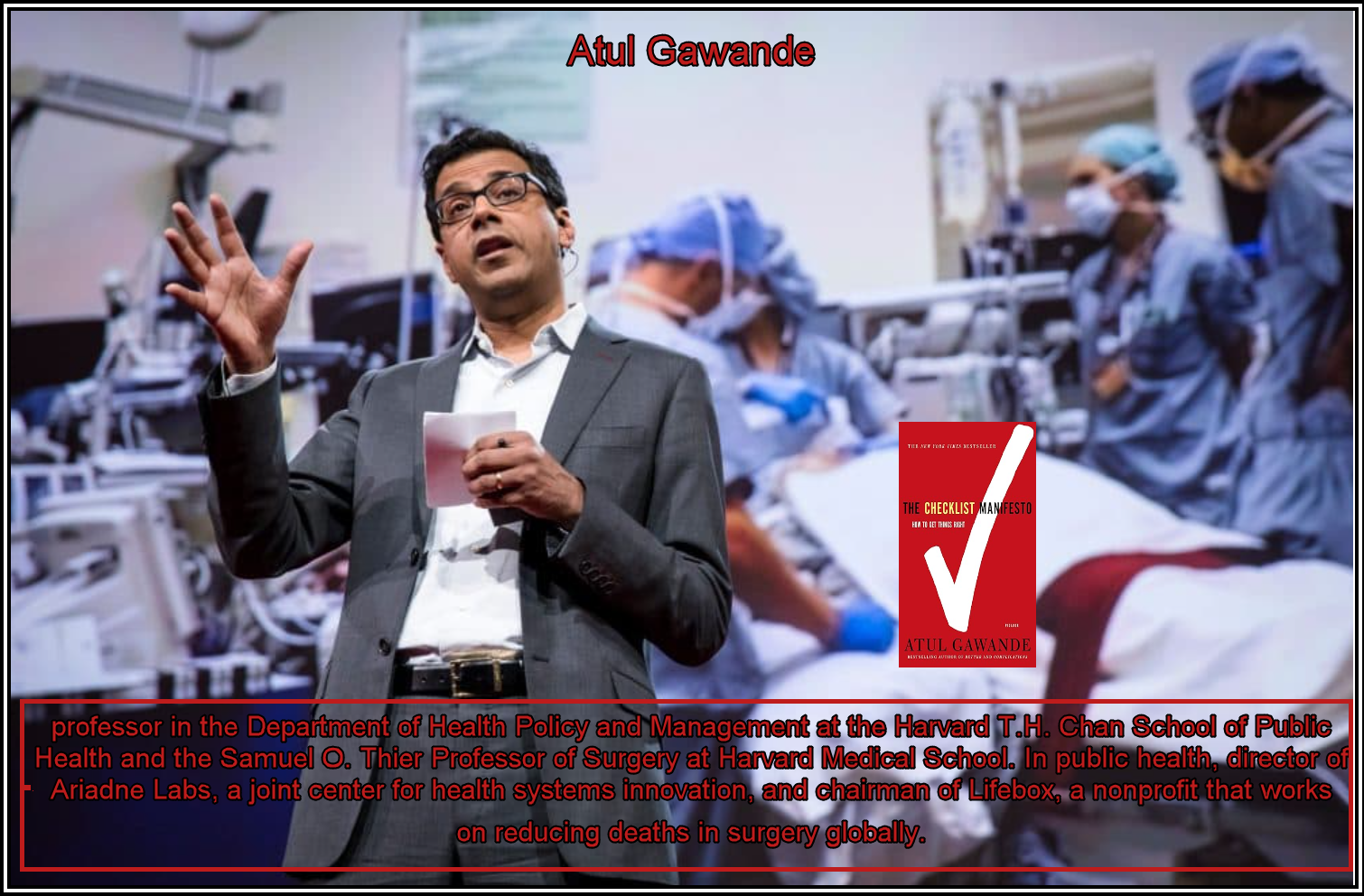
Dr. Gawande, who now works at Brigham and Women’s hospital in Boston, expanded on the idea in his 2009 book, “The Checklist Manifesto: How to Get Things Right.” The year prior, aviation and medical safety expert John Nance published “Why Hospitals Should Fly: The Ultimate Flight Plan to Patient Safety and Quality Care.”
Despite the interest in how hospitals can transfer those teachings, healthcare safety advancements have lagged behind that of the aviation industry.
If the airline industry made as many mistakes as healthcare does, there would be about 460 plane crashes every day, according to Jimmy Chung, MD, chief medical officer of Advantus Health Partners, a group purchasing organization formed by Bon Secours Mercy Health.
“Just looking at how many airline’s flights are taken every day, imagine if 460 of them crashed every day,” said Dr. Chung, who compared the two industries in a 2021 opinion article. “We would not stand for it.”
Becker’s spoke with healthcare and aviation experts about why this comparison is so popular, how far the metaphor stretches and its potential pitfalls.
The culture problem
Hospital leaders and industry experts pointed to a crucial difference between healthcare and airlines: The former has a blame culture directed at individual actions; the latter targets systematic issues after a mistake is made, known as a “just culture” — but the aviation industry wasn’t always this way.
When commercial aviation began expanding in the 1950s and ’60s, many pilots were ex-air force and unfamiliar with interacting with crew or passengers, according to Niall Downey, MD.
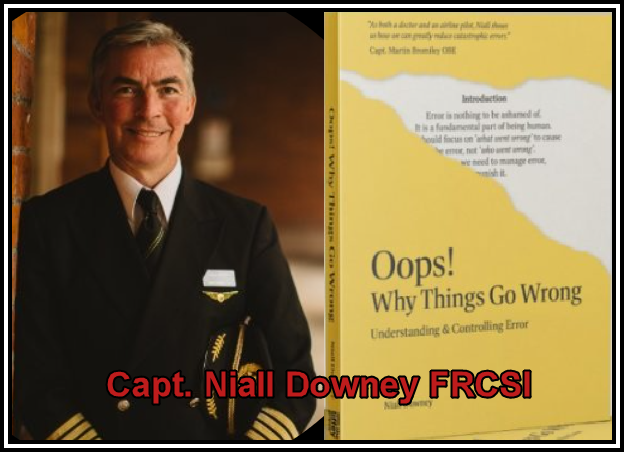
“The whole mentality then was different,” said Dr. Downey, a captain for Aer Lingus and a former cardiothoracic surgeon. Co-pilots did not feel safe speaking up or were dismissed when they did.
In 1977, airlines deviated from this culture of “name, blame, shame, retrain,” according to Dr. Downey.
Two Boeing 747 jets collided on a runway on a Spanish island off Africa’s west coast killing 583 people in March 1977 — making it the deadliest accident in aviation history, according to the Federal Aviation Administration. The event, called the Tenerife airport disaster, spurred an industrywide revolution in safety and a culture reboot in which pilots are not disciplined or fired for small errors.
“The trajectory of the number of deaths in commercial jet aviation, back in 1977, was about 3,000 deaths per year,” Dr. Downey said. “The amount of aviation has gone up 9-fold. We should be looking at about 27,000 deaths per year in aviation. We’re actually looking at about 1,000 — so it’s about a 96% improvement. Healthcare would like to be able to do that, but they don’t like the approach that it’s going to involve to actually get there.”
Dr. Downey is the managing director of Frameworkhealth, a company he founded in 2011 that translates aviation’s success for healthcare.
Teodor Grantcharov, MD, PhD, associate chief quality officer for safety and innovation at Stanford Medicine; Deborah Rhodes, MD, enterprise chief quality officer of Yale Medicine; and Dr. Downey all said the DECADES LONG BLAME CULTURE in medicine is the biggest barrier to elevating patient safety.
In hospitals, a culture of silence and blame can fester. Whistleblowers on safety issues have accused their former employers of ignoring concerns and forcing them to leave.
Some front-line healthcare workers have also expressed fear of criminalization for admitting to medical errors in the wake of RaDonda Vaught’s conviction. In 2022, the American Nurses Association said Ms. Vaught’s case, which made national headlines, could have a “chilling effect” on medical error reporting and process improvement in healthcare.
“Healthcare has had a blame culture for so long that the staff actually apply it to themselves,” Dr. Downey, who was a cardiac surgeon for about a decade, said. “When they make a mistake, they blame themselves as well.”
Many hospitals and health systems nationwide are working to build a just culture in healthcare, including Johnson City, Tenn.-based Ballad Health.
“For people who may be so-called low on the hierarchical command of things […] and they are afraid of the physician’s anger or wrath, they’re not able to point that error up,” said Amit Vashist, MD, senior vice president and chief clinical officer of Ballad. “How do we create that psychological safety?”
HOW HEALTHCARE IS REPLICATING AVIATION
Other than rerouting workplace cultures away from blame and shame, hospital leaders are also investing in other aviation-influenced strategies and procedures.
One example is the flight recording device and cockpit voice recorder placed in every airplane. The devices are known as “BLACK BOXES” despite their orange color, which help emergency response crews find them in a wreck site.
Dr. Grantcharov drew inspiration from the device to launch “Operation Black Box.” His invention, the OR Black Box, is made of sensors and data recorders that collect information. AI analyzes the data and videos — which blur faces, distort voices and are deleted after 30 days — to find inefficiencies.
The product also helps increase the exchange of information. Dr. Grantcharov said he might do the same operations as a handful of other surgeons at Palo Alto, Calif.-based Stanford Medicine, but successes and failures aren’t shared with one another.
“The surgical operating room is probably one of the most secretive environments in society,” Dr. Grantcharov said.

In October 2022, Stanford Hospital installed his black boxes in four operating rooms.
Mistakes are often kept to the individual or team level in healthcare, according to Dr. Downey. If an accident happens at an airline, though, “the entire industry knows what happens,” Dr. Grantcharov said.
The international aviation industry meets a few times a year to share problems and solutions, as well as learn from one another’s mistakes. One of these events is called Aviation Safety InfoShare, which dials in on systemwide best practices for safety.
Healthcare does not have a comparable event.
At healthcare conferences, “you still see different institutions talking about how innovative they are because they do things differently and they use technology differently,” Dr. Chung said.
In medical school and residencies, physicians are taught to be independent and think outside the box: “No surgeon has ever become famous by saying, ‘Hey, I do things the exact same way as everyone else,'” he said. “Physicians aren’t trained to be standardized.”
Without a regulatory standard for the industry, hospitals and systems are working to create archetypes to improve patient care — similar to the same checklists used by aircraft workers.
Dr. Rhodes, who works at New Haven, Conn.-based Yale Medicine, is tackling clinical variation at her organization. Over the last decade, she has been developing clinical pathways for hundreds of conditions.
For example, EHRs for patients with chronic obstructive pulmonary disease will pull up the COPD pathway, which tells Yale clinicians the standard for confirming a diagnosis, how to manage treatment, when a patient can be discharged, and it provides post-discharge resources.
This pathway is built from expert consensus, exhaustive literature review and lengthy industry guidelines.
“I can read [COPD guidelines] in April, but will I have a detailed recall of all the steps in a 120-page guideline in September? No, I won’t,” she said. “That’s why we have to bake that.”
Yale Medicine has been using the pathways for about three years, and in an “extraordinary” clinician uptake, they’re now used 30,000 times a month, according to Dr. Rhodes.
Patients aren’t planes, but the metaphor doesn’t crumble
Many hospital executives told Becker’s the comparison isn’t a 1:1 ratio. Physicians aren’t pilots, patients aren’t planes, hospitals aren’t airports, et cetera.
“THERE’S A FINITE NUMBER OF DIFFERENT THINGS THAT CAN GO AWRY WHEN YOU’RE FLYING A PLANE AND THERE’S AN INFINITE NUMBER OF THINGS THAT CAN GO AWRY IN MEDICINE,” Dr. Rhodes said.
Jonathan Perlin, MD, PhD, president and CEO of The Joint Commission Enterprise, echoed this.
“I think there is much to learn from aviation, but that in a patient’s journey, unlike that of an aircraft, the destination may not be known,” Dr. Perlin told Becker’s before boarding a plane. “Thus, healthcare is more complex.”
Another crack in the comparison is a glorification of airline safety. In the last decade, there have been more than twice as many near misses between commercial flights than years past, according to The New York Times. Experts have said the national shortage of air traffic controllers is a main reason for this.
Those who dismiss the metaphor altogether, though, don’t understand the role of airline captains, according to Dr. Downey, who has been in the airline business for 24 years.
One sick passenger on an international flight of 300 people can cost up to $500,000, he said. If he’s flying from Dublin to Chicago, for example, and has to divert to Keflavík airport in Iceland for a few hours because of a sick passenger, the airline then has to cover hotel rooms for the 300 people on the plane and the 300 waiting in Chicago to fly home.
It can then take days to resolve a ripple effect of disturbances in an airline’s schedule.
“They assume an airline captain flies the plane. That’s the least part of my job,” he said. “A lot of what we do is try to juggle operations and look at long-time consequences of small decisions. Exact same as healthcare.”
Dr. Grantcharov and Dr. Downey agreed that HEALTHCARE IS FAR FROM FULLY EMBRACING THE AVIATION INDUSTRY’S TECHNIQUES, but a few hospitals and health systems have steadily worked to manifest the idea into reality.
The younger generations entering healthcare are more likely to value standardization over autonomy, Dr. Rhodes said, which can help quell the blame culture.
“Things are getting better. With this generation, I think we are going to get this across the line,” Dr. Downey said. “But, it’s a hard sell.”

Copyright © 2023 Becker’s Healthcare. All Rights Reserved. Privacy Policy. Cookie Policy. Linking and Reprinting Policy.